COVID Infection Rates Have Plateaued at a High Level
Although forty percent of eligible Americans have received at least one COVID vaccine injection, the number of cases has plateaued as of late April. The most recent available data shows that the number of new infections on April 20th was 20 per hundred thousand residents at the national level compared with 12 per hundred thousand on September 1st, 2020.
The number of new cases per day late in April averaged about 60,000. At the current rate, the nation would see an additional 21,500,000 COVID-19 infections in the coming year. The death rate for those who tested positive for COVID-19 in December 2020 was 1.7%. At that rate, the nation could have more than 360,000 additional deaths in the next twelve months, on top of the 570,000 who have already died.

New positive COVID-19 test results show that community COVID infection rates in New York State have been higher than the national rate since January. Since the beginning of April, New York’s infection rate relative to the rest of the nation has improved, however, declining from 37 per hundred thousand on April 1st to 29 on April 24th.
Several factors could be contributing to the current high levels of COVID spread. Infection rates are higher when people are in close contact in indoor spaces. The infection spikes during the holiday season may have been caused by family gatherings at Thanksgiving and Christmas. Many of the states with high rates of infections during the winter, like New York, have cold climates that prevent people from gathering and dining outdoors. Additionally, the spread of COVID variants with higher transmissibility rates, such as the British variant B.1.1.7, which is 60% more transmissible and has a 67% higher mortality rate, has increased case counts. Given these factors, can we measure the impact of COVID vaccinations on infections and death rates?
Age as a Risk Factor
Because of the relatively small percentage of all residents who have been fully vaccinated – 25% – and the influence of factors like seasonality and COVID variants, it is difficult to determine whether vaccinations have reduced the rate of community infection or deaths using aggregate data. But, because the United States has employed a strategy of immunizing at-risk groups first, particularly the elderly, we can compare rates of infections and deaths between groups with differing vaccination rates.

The risks associated with contracting COVID-19 were not overstated. The risk of hospitalization for COVID-19 is high – particularly for those aged 50 and above. Seven percent of those aged 50-65 who had been diagnosed with COVID were hospitalized in January. For the population aged 65-74, 16% required hospitalization. Nearly 40% of those aged 85 or more were hospitalized.

Deaths are another particularly concerning consequence of COVID infections. The relationship between age and COVID-related deaths is even stronger than for hospitalization rates. Only about 0.05% of those 18-34 who tested positive for COVID-19 in October 2020 and January 2021 died of COVID-related causes. Death risk increased rapidly with age. Slightly more than one percent of those aged 55-64 who were diagnosed died, while more than 5% of those between 65 and 79 died. The relative risk of death for those aged 65-79 is 125 times higher than for the 18-34 age group. For those aged 80 or more, the picture was even worse. Almost one out of five who tested positive for COVID-19 in October 2020, and January 2021 died.
For a person aged 55 to 64 or more, who would not seek to avoid an infection that killed 12 of every thousand diagnosed people? For those aged 65-79, the numbers are even worse – 53 of every thousand people diagnosed last fall and winter died, while for those aged 80 or more, more than 180 of every thousand people diagnosed died of this single cause. Given the high levels of hospitalization and death associated with COVID, the measures put in place by public health officials to control the disease – social distancing, masking, and handwashing – seem reasonable.
Vaccination Rates

Although recent polling data shows that many Americans are skeptical of COVID vaccinations, seniors have been highly receptive. More than 80% of those 65 or older had received at least one dose by April 20th. Sixty-six percent had been fully vaccinated. The vaccination of the elderly population ramped up rapidly, beginning in mid-January. COVID vaccines were not made generally available to the adult population until April. Because vaccination rates for seniors are much higher than for younger age groups, by comparing changes in infection and death rates among the groups, we can discern the impact of the vaccine.

By March 27th, more than 70% of those aged 65 or older had received at least one shot, while about half had been fully vaccinated. People in younger age groups were far less likely to be vaccinated as of that date – with less than 20% of those groups fully vaccinated. More recent data is available but was not used for this research because of potential errors associated with delays in reporting and compilation of case, hospitalization and death data.
Positive Test Rates
If the COVID vaccine had reduced the number of infections and deaths, even at this point, when only about half of those over 65 had completed required inoculations, lower rates of illness and deaths for seniors compared to younger groups with lower rates of vaccinations should be evident.

Although the rate of new COVID cases per hundred thousand residents for each age group was lower for the week ending March 27th than the rate in October 2020, the decrease was substantially greater for those who are 65 years old or older. Case rates for seniors dropped by 49%. The largest decline for younger age groups – those who are 55 to 64 – was 28%.
COVID Related Fatality Rates
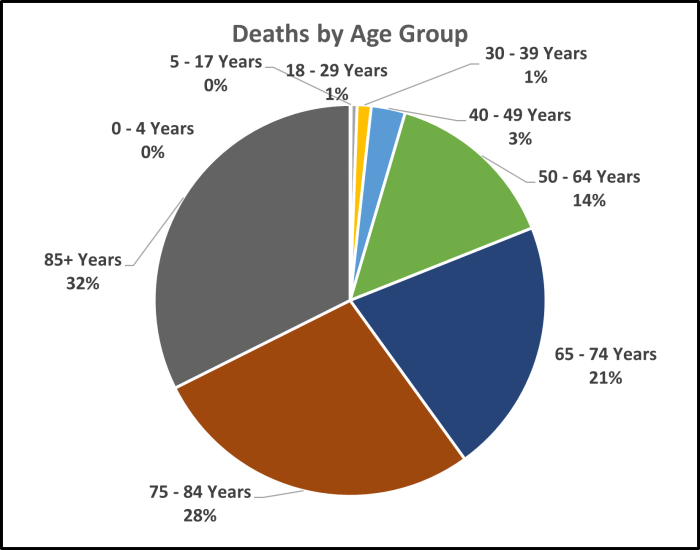
Because the risk of death from COVID is strongly related to age, the number of deaths of older people is much greater than among younger age groups. Ninety-six percent of deaths from COVID were among people aged 50 or older. Eighty-one percent were aged 65 or higher.

Since mid-January, when the elderly population began to be vaccinated on a mass scale, deaths have dropped sharply, with the rate of deaths among the elderly showing the sharpest decrease. Despite the overall drop in the number of weekly deaths since the beginning of 2021, the weekly rate of COVID-related deaths among those aged 18-34, though very small, has remained nearly constant. For those aged 55-64, there has been a somewhat larger decrease – about five deaths per hundred thousand people. The drop for those aged 65 to 70 has been much larger – about 16 per thousand. For those aged 80 or older, the decrease was 64 per hundred thousand.

While the number of deaths per week decreased between January 2nd and March 27th, the decrease was primarily among those 55 years old or older – 16,000 of 17,200. Although the decline in the rate of deaths was greatest among the highly vaccinated elderly population, we cannot attribute all of the reduction to COVID vaccinations. Other factors, including the end of the holiday season and warmer weather, particularly in the South and West, have also contributed to the reduction in deaths.
Conclusions
The impact of the COVID-19 pandemic has been sobering. More than 570,000 Americans have died. Many more have been hospitalized. Prior to the development and deployment of vaccines, the only measures available to control its spread were those imposed in 1918 against the Spanish Flu- primarily social distancing and masking – measures that physically reduced the likelihood of spread from infected people.
Although the American population widely accepted these measures, infection rates peaked in the Winter of 2020. More than 300,000 people have died from COVID-related causes since Thanksgiving. During that time, one of every thirteen people between 55 and 64 years old diagnosed with COVID was hospitalized. Twelve of every thousand people who tested positive in that age group died. For those aged 65-74, one in six diagnosed were hospitalized, and one in 20 died.
The development of vaccines to control the spread of COVID marks a fundamental advance in preventing the spread. The vaccines reduced the risk of infection by reducing the likelihood that those exposed could be infected by as much as 90%. Equally important, recent reports indicate that the Moderna and Pfizer vaccines reduce the transmission of disease from vaccinated people.
According to the report, “We clearly showed in our study that if you were at least 14 days out from your first shot, you had 80 percent protection” from infection, says Jeff Burgess, associate dean for research at the Mel and Enid Zuckerman College of Public Health at the University of Arizona in Tucson. The study is part of a growing body of evidence suggesting that the vaccines not only reduce the risk of getting seriously ill with COVID-19 but can prevent catching the virus in the first place.
“If you can’t get infected, you can’t infect anyone else, which means the vaccines can reduce transmission as well as the disease,” says Marm Kilpatrick, an infectious diseases researcher at the University of California, Santa Cruz, who was not involved in the study.
Early evidence suggests that the roll-out of vaccines has substantially reduced hospitalizations and deaths in the elderly. With more than 80% of deaths last fall and winter in people aged 65 years old or more, the fact that 80% of that population has been vaccinated is good news. Between early January and the end of March, the number of COVID-related deaths of people aged over 65 dropped by 93%, a greater decline than for other ages.
The number of positive test results remains high – about 60,000 daily. Deaths are lower, but we could lose another 240,000 people in the coming year, even at the current rate. With only about 40% of the nation’s population vaccinated, we have a long way to go before infections and deaths reach a low level.
To date, the demand for vaccinations has been high, with demand exceeding supply. But there is evidence that we are rapidly moving towards the point where the nation’s capacity to vaccinate people will exceed the demand for vaccines. As of April 24th, 51% of the eligible population has been vaccinated, but a significant portion – 37%, according to the most recent Kaiser Family Foundation poll – does not plan to get vaccinated soon. If 37% of the population remains unvaccinated, the nation will not soon reach so-called “herd immunity”. Infection rates would stay at levels requiring social distancing, mask-wearing, and capacity controls in public environments.
Reaching the remaining unvaccinated population is made more difficult because much of it comprises the age groups that are at relatively low risk. In fact, the risk is not negligible – even for those aged 25-34, six of every ten thousand people who were diagnosed with COVID die. For those aged 35 to 43, 14 of every ten thousand COVID positive people die. Thirteen of every ten thousand people diagnosed with COVID in their 20s have been hospitalized. For people in their 40s, 30 of every ten thousand required hospitalization. Some younger people do not believe they are at risk from COVID, even as the average age of those hospitalized drops.
The Biden administration has seen high levels of public approval for its efforts to control the spread of COVID-19. The rapid roll-out of COVID vaccines accounts for much of the positive response. But, the next phase of the roll-out will be more challenging. Unless the views of some who are skeptical of COVID vaccines can be swayed, the nation will face a choice between limits on social activities – dining, amusements, concerts, and the like – and continued COVID-related hospitalizations and deaths.
I find John’s work to be the most even handed and evidence based available on this and other controversial matters.
Thank you very much.
John